What Is NIPT? Overview for Expectant Mothers
Mar 24, 2025
Rita Singha
Pregnancy Health
Non-Invasive Prenatal Testing (NIPT) is a safe blood test that screens for certain genetic conditions in a baby as early as 10 weeks into pregnancy. It works by analyzing DNA from the placenta found in the mother’s blood and has no physical risk to the baby. Here’s what you need to know:
What It Screens For: Common chromosomal conditions like Down syndrome (Trisomy 21), Edwards syndrome (Trisomy 18), and Patau syndrome (Trisomy 13). It can also determine fetal sex and detect some sex chromosome anomalies.
Accuracy: About 99% for Down syndrome, significantly reducing false positives compared to older methods.
Who Should Consider It: While recommended for all pregnant women, it’s especially useful for those over 35, with a family history of genetic conditions, or abnormal earlier screenings.
Limitations: NIPT is a screening tool, not a diagnostic test. High-risk results require follow-up testing like amniocentesis or CVS for confirmation.
This test is a reliable option for early insights into your baby’s health, but it’s important to discuss your results and next steps with your healthcare provider.
What Is NIPT?
Definition and Purpose
Non-Invasive Prenatal Testing (NIPT), also called cell-free DNA screening, is a blood test designed to analyze DNA fragments from the placenta circulating in the mother’s blood. These DNA fragments carry genetic information that can help determine the risk of certain chromosomal abnormalities in the baby.
NIPT primarily screens for conditions like Trisomy 21 (Down syndrome), Trisomy 18, and Trisomy 13. Additionally, it can provide insights into fetal sex, Rh status, and some sex chromosome anomalies. This test allows expectant mothers to take proactive steps in managing prenatal care.
It’s important to note that NIPT is a screening tool, not a diagnostic test. This means it provides a risk estimate rather than a definitive diagnosis. If the results indicate a high risk, follow-up diagnostic procedures like amniocentesis or chorionic villus sampling (CVS) are needed to confirm the findings.
NIPT boasts high accuracy with minimal false positives - typically 1–3%, compared to 2–7% in traditional screening methods. This not only reduces unnecessary stress but also limits the need for additional testing, all without posing any risk to the baby.
Understanding what NIPT evaluates can help you decide if this test is right for your pregnancy.
Who Should Consider NIPT?
With its high level of accuracy and safety, NIPT is now recommended for a broader group of expectant mothers. Both the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) advise offering NIPT to all pregnant women, regardless of age or baseline risk. This universal recommendation highlights the test’s reliability and non-invasive nature.
While NIPT is now an option for all pregnancies, certain groups may benefit even more. For instance, women aged 35 or older face a higher likelihood of chromosomal abnormalities, making the test particularly reassuring. Similarly, those with a personal or family history of genetic conditions or abnormal results from earlier screenings may find NIPT especially useful.
Before opting for NIPT, it’s a good idea to check with your insurance provider. Many plans now cover the test for all pregnancies, though some may require specific risk factors for full coverage. Consulting with a genetic counselor can also help you better understand the test results and decide if NIPT aligns with your needs.
How Does NIPT Work?
The Testing Procedure
NIPT begins with a simple blood draw from your arm, usually taking just a few minutes at your healthcare provider’s office or a lab.
After your sample is collected, it’s sent to a specialized lab where the plasma - the liquid part of your blood - is separated. This plasma contains tiny fragments of cell-free DNA (cfDNA), each less than 200 base pairs long, that circulate in your bloodstream. During pregnancy, some of this cfDNA comes from the placenta, which closely mirrors your baby’s genetic material. This makes it an excellent source for genetic screening.
The lab uses next-generation sequencing (NGS) to examine these DNA fragments. Depending on the test panel, the lab selects the most appropriate method for analyzing the cfDNA. For reliable results, the "fetal fraction" (the percentage of placental DNA in your blood) must be at least 4%, which is typically reached by the 10th week of pregnancy. Results are usually available within one to two weeks, providing a clear and accurate assessment of your baby’s genetic profile.
What NIPT Screens For
After the testing process, NIPT focuses on detecting specific chromosomal conditions. Standard panels primarily screen for three conditions: Trisomy 21 (Down syndrome), Trisomy 18 (Edwards syndrome), and Trisomy 13 (Patau syndrome). By counting the DNA fragments from each chromosome, the test identifies if there’s an excess of DNA from one chromosome, which could indicate a higher risk of that particular trisomy.
NIPT is highly sensitive, especially for Down syndrome, with about 99% accuracy. It can also identify your baby’s biological sex with over 99.99% accuracy and detect sex chromosome abnormalities such as Turner syndrome (45,X) or Klinefelter syndrome (47,XXY). Some tests go further, screening for microdeletions - small missing pieces of chromosomes like the 22q11.2 deletion syndrome (DiGeorge syndrome). However, these microdeletion results are less reliable, with up to 85% of positive findings being false positives.
"NIPT is considered noninvasive because it requires drawing blood only from the pregnant woman and does not pose any risk to the fetus." - MedlinePlus Genetics
Since screening panels differ between laboratories, it’s essential to consult your healthcare provider or a genetic counselor to understand what your specific test covers and the conditions being evaluated.
What is NIPT Testing in Pregnancy? | Genetic Counselor Explains
Benefits and Limitations of NIPT
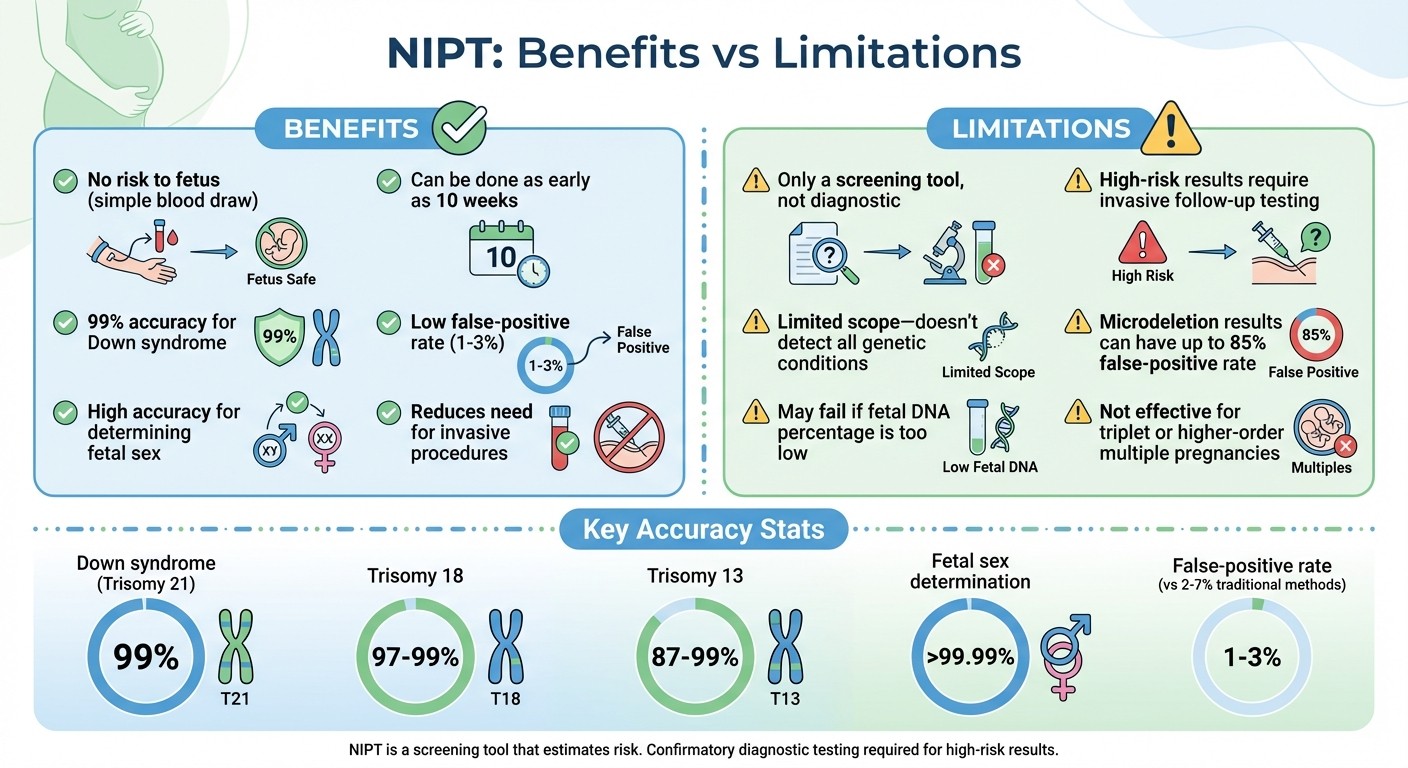
NIPT Benefits vs Limitations: Complete Comparison for Expectant Mothers
Benefits of NIPT
NIPT offers several advantages for expectant mothers. It requires just a simple blood draw, which means there’s no risk of miscarriage. Plus, you can take the test as early as 10 weeks into your pregnancy.
One of the standout features of NIPT is its high accuracy for detecting common chromosomal conditions. For Down syndrome, the accuracy is an impressive 99%, while Trisomy 18 results range between 97–99%, and Trisomy 13 between 87–99%. This precision significantly reduces false alarms compared to traditional screening methods, which typically have false-positive rates of 2–7%. According to the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM), NIPT offers "the highest detection rate and lowest false positive rate for the common aneuploidies regardless of maternal age or baseline risk, of all screening options."
While these benefits are compelling, it’s important to weigh them against the test's limitations.
Limitations and Considerations
NIPT is a screening tool, meaning it estimates risk rather than providing a definitive diagnosis. If the test indicates a high risk, confirmatory invasive procedures like amniocentesis are necessary. Additionally, NIPT has a limited scope - it does not detect conditions like neural tube defects, single-gene disorders, or autism.
The test analyzes DNA from the placenta, which can sometimes lead to results that reflect chromosomal changes in the placenta rather than the fetus. Factors like maternal obesity, twin pregnancies, or a low fetal DNA percentage (less than 4%) can also impact the test’s accuracy.
Pros and Cons Comparison
Here’s a quick breakdown of NIPT’s strengths and weaknesses:
Advantages | Disadvantages |
|---|---|
No risk to the fetus (simple blood draw) | Only a screening tool, not diagnostic |
Can be done as early as 10 weeks | High-risk results require invasive follow-up testing |
99% accuracy for Down syndrome | Limited scope - doesn’t detect all genetic conditions |
Low false-positive rate (1–3%) | Microdeletion results can have up to an 85% false-positive rate |
High accuracy for determining fetal sex | May fail if fetal DNA percentage is too low |
Reduces need for invasive procedures | Not effective for triplet or higher-order multiple pregnancies |
Understanding these points can help you make informed decisions about when to take the test and how to prepare for it.
When Should You Consider NIPT?
Best Timing for the Test
NIPT (Non-Invasive Prenatal Testing) can be done as early as 10 weeks into pregnancy and remains an option throughout. Why 10 weeks? Before this point, there usually isn’t enough fetal DNA circulating in your bloodstream for accurate results. The test works by analyzing cell-free DNA fragments from the placenta, and to ensure accuracy, the fetal fraction (the percentage of placental DNA) typically needs to be above 4%.
Taking the test too early increases the chances of getting no result or even a false negative due to insufficient fetal DNA. As noted by ACOG and SMFM, "Cell‐free DNA screening [NIPT] is the most sensitive and specific screening test for the common fetal aneuploidies (trisomies 21, 13, and 18) and can be performed at any time after 9‑10 weeks of gestation." - ACOG/SMFM
By following these timing guidelines, you can ensure the test’s accuracy, while your personal circumstances may further influence the recommendation.
Factors to Consider
Beyond timing, your individual risk factors play a role in deciding whether NIPT is right for you. Current recommendations suggest NIPT for all pregnancies, regardless of traditional risk factors.
That said, your doctor might prioritize NIPT if you fall under certain categories, such as being of advanced maternal age, having a history of chromosomal abnormalities, or receiving abnormal results from earlier screenings. Interestingly, 70% of Down syndrome cases occur in pregnancies of women under 35, highlighting the importance of universal screening.
Don’t forget to check your insurance coverage, and keep in mind that if follow-up diagnostic testing is needed, it carries a small risk of miscarriage.
How to Prepare for NIPT and Understand Results
Once you’re familiar with how NIPT works and what it screens for, the next step is knowing how to get ready for the test and make sense of the results.
Preparing for the Test
Here’s the easy part: no special prep is needed for NIPT. Unlike some medical tests, there’s no fasting or changes to your routine. It’s as simple as a blood draw from your arm - similar to standard bloodwork you may have had before.
Before your test, talk to your healthcare provider or genetic counselor about what the test covers and what the results could mean. If you’d like to find out your baby’s sex, let your provider know, or mention if you’d rather keep it a surprise. It’s also smart to check with your insurance company ahead of time, as coverage can vary depending on your plan and whether your pregnancy is classified as high-risk.
Keep in mind, certain factors like maternal obesity or testing too close to 10 weeks of pregnancy might result in insufficient fetal DNA in the sample. If this happens, you may need a second blood draw. Being informed about these details helps you feel more prepared and confident when it’s time to review your results.
Understanding Your Results
You can expect your results within 10 to 14 days, and they’ll fall into one of three categories: negative (low risk), positive (high risk), or inconclusive. A key number to look for is the fetal fraction, which is the percentage of fetal DNA in your blood. For the results to be reliable, this number needs to be above 4%. If it’s lower, retesting might be necessary.
"NIPT is a screening test, which means that it will not give a definitive answer about whether or not a fetus has a genetic condition. The test can only estimate whether the risk of having certain conditions is increased or decreased." - MedlinePlus
If your results indicate high risk, try to stay calm. It’s important to remember that NIPT is a screening tool, not a diagnostic test. For example, high-risk results are confirmed as true positives in about 91% of cases for Down syndrome, 84% for Edwards syndrome, and 87% for Patau syndrome. The next step is to meet with your healthcare provider or genetic counselor to explore diagnostic options.
Diagnostic tests like chorionic villus sampling (CVS) (performed between 10–13 weeks) or amniocentesis (after 15 weeks) can confirm the results. These procedures come with a small risk of miscarriage - about 1 in 455 for CVS and 1 in 900 for amniocentesis - but they provide definitive answers. Be sure to ask your provider about the Positive Predictive Value (PPV) for your specific situation, as this will give you a clearer picture of how accurate a high-risk result is based on factors like your age and medical history.
Conclusion
NIPT is a safe and effective way to screen for chromosomal conditions like Down, Edwards, and Patau syndromes, with an accuracy rate of about 99% for Down syndrome. This noninvasive test has become a reliable option for pregnant women, regardless of their risk level, as it only requires a simple blood draw and poses no physical risk to the pregnancy.
It’s important to remember that NIPT is a screening tool designed to estimate risk. If the results indicate a high risk, follow-up diagnostic tests like amniocentesis or CVS are necessary to confirm the findings before making any major decisions. The American College of Obstetricians and Gynecologists highlights the need for proper follow-up and patient education:
"All patients should have the opportunity to discuss screening and diagnostic testing options with their clinician to understand the options and risks and benefits of available screening and testing." - American College of Obstetricians and Gynecologists (ACOG)
While NIPT offers high detection rates and fewer false positives compared to traditional screening methods, it does have its limitations. It can be performed as early as 10 weeks into pregnancy but doesn’t screen for all genetic conditions or physical birth defects. This makes it essential to have an in-depth discussion with your OB-GYN or genetic counselor to understand how this test fits into your prenatal care.
Your healthcare provider can help you interpret the results, explore insurance coverage, and plan next steps if needed. An informed decision begins with an open, honest conversation with your care team.
FAQs
What can cause an inconclusive NIPT result?
An inconclusive NIPT result can happen when there’s a low fetal fraction, which is often just a normal variation in early pregnancy. Sometimes, maternal factors like higher body weight or a limited amount of fetal DNA from the placenta can also make it challenging to analyze chromosomal proportions accurately. While this isn’t usually a reason to worry, it might mean a repeat test or additional follow-up is needed.
How likely is a high-risk NIPT result to be correct?
A high-risk NIPT result is incredibly precise, identifying approximately 99% of chromosomal abnormalities, such as Down syndrome. Despite this accuracy, it’s important to remember that NIPT is a screening tool, not a diagnostic one. To confirm the result, further diagnostic testing is required.
Do I still need an ultrasound or other prenatal screenings after NIPT?
Yes, ultrasounds and other prenatal screenings are often recommended following NIPT. These tests play a crucial role in monitoring the baby’s development and detecting any concerns that genetic screenings might miss. Be sure to discuss your options with your healthcare provider to receive guidance tailored to your situation.
